|
Every day, tens of thousands of elderly Americans in nursing
homes are chemically restrained by powerful, dangerous,
and expensive antipsychotic drugs. Prescribed to "treat"
people with Alzheimer's and other dementias,
antipsychotics have no therapeutic value for most of these
vulnerable patients. They are used, against best evidence,
for extended periods; risk fatal side effects; and are usually
dispensed "off-label"* since, in almost every instance, they
lack FDA approval for treating dementia.
The British Medical Journal recommends that for people
with dementia, "antipsychotics should be carefully targeted,
time limited, and reserved for severe and distressing
symptoms after careful assessment of risk and benefit."
Nonetheless they have become a drug of first resort. In
2010, almost 40 percent of nursing home residents with
signs of dementia, but no diagnosis of psychosis, got
antipsychotics – often at higher dosages and for longer
durations than recommended.
If you know an Alzheimer's victim, you will likely have
watched a previously vital person buried alive in confusion,
oblivion, hopelessness and fear. Patients who have lost
contact with language, social interactions, and their own
minds and memories are often depressed and agitated.
Some, unable to articulate their suffering, are in constant
pain because of untreated conditions. Families, doctors,
and caregivers are desperate for relief, but there is no
chemical fix.
In most cases, antipsychotics simply control problematic
behavior by doping patients into docility. They can then be
more cheaply warehoused in inadequately staffed and
underfunded institutions.
What patients need instead, is "consistent staff
assignments, increased exercise or time outdoors,
monitoring and managing acute and chronic pain, and
planning individualized activities," according to according
to the Centers for Medicare and Medicaid Services (CMS).
And trained caregivers. In one nursing home with largely
untrained staff, 80 percent of patients were drugged with
antipsychotics, the Boston Globe noted.**
Political will is also essential. Between 2008 and 2011,
Britain's public health service acknowledged the problem,
and more than halved antipsychotic prescriptions for
dementia patients.
America – with an $18.2 billion antipsychotics market as of
2011 -- has lagged in educating and regulating doctors,
nursing home administrators, and pharmacists. CMS's goal
for 2012 is a 15 percent reduction. As for BigPharma, it
games the system, reaps vast profits, and when caught in
criminal activity, pays fines as a cost of doing business.
In 2009 Eli Lilly pled guilty to a misdemeanor criminal
charge and paid $1.4 billion for targeting doctors at
nursing homes and assisted living facilities to prescribe its
antipsychotic olanzapine off-label to dementia patients.
This year, Omnicare Inc., which provides pharmacy-related
services to long-term care facilities, accepted a $2.2 billion
settlement for taking kickbacks from Johnson & Johnson for
recommending J&J drugs, including its antipsychotic
Risperdal, at the nursing homes it serviced.
With research showing that some antipsychotics doubled
the risk of death, the FDA issued a "black-box" warning -- its
strongest alert, reflecting hard evidence that a drug carries
a significant risk of serious or life-threatening adverse
effects. Side effects of antipsychotics include excessive
sedation, dizziness leading to falls, tremors, social
withdrawal, accelerated cognitive decline, as well as more
strokes, cardiac events, embolisms, some of which lead to
death.
Facing increased vigilance, Abbott Laboratories got clever.
It pushed Depakote--not technically an antipsychotic--as an
off-label treatment for dementia. From 1998 to 2006,
Abbott maintained a sales force specifically trained to
market Depakote in nursing homes to "control of agitation
and aggression in elderly dementia patients, despite the
absence of credible scientific evidence that Depakote was
safe and effective for that use," the the Justice Department
charged in May 2012. Abbott bribed long-term care
pharmacy providers with million in "rebates based on
increases in the use of Depakote in nursing homes," the DoJ
said. This year Abbot pleaded guilty, and agreed to pay
$1.5 billion. Its 2011 earnings were $39 billion; Lilly's
topped $24 billion.
Ultimately, tax dollars feed those profits, since Medicaid,
Medicare and veterans benefits pay for many of the meds
taken by America's 5.4 million Alzheimer's patients.
Dementia patients, however, pay in pain, stupor and death.
"Excessive prescription of antipsychotic drugs in nursing
homes is elder abuse plain and simple," said Sen. Richard
Blumenthal (D-Conn.) in a press release. "It is chemical
restraint, as pernicious and predatory as unnecessary
physical restraint."
Since fines fail to deter BigPharma crime, perhaps we should
chemically restrain the executives responsible with their
own drugs, or physically restrain them with prison
sentences.
-------------------------------
*Off-label: The FDA approves drugs only for the purpose for
which they were tested. Legally, drug companies can
promote the drugs only for the FDA-approved purpose.
Doctors, however, can legally prescribe drugs "off label" for
conditions not covered by the FDA approval.
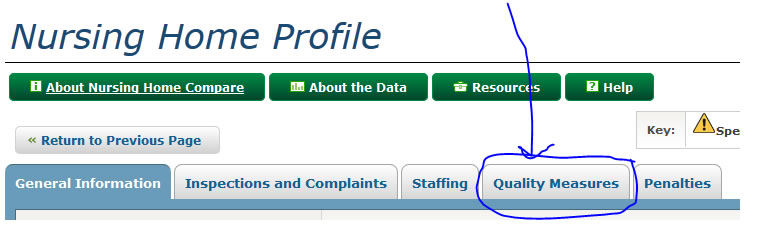
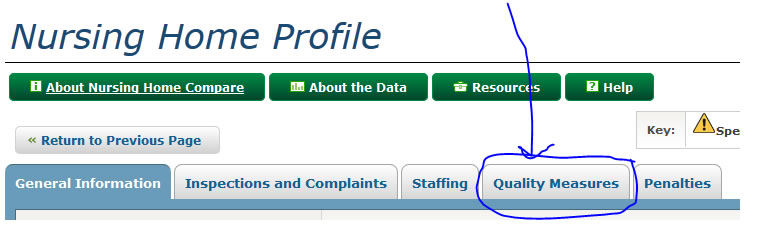
**For a detailed assessment of nursing homes in your area,
including information on use of antipsychotics, see:
http://www.medicare.gov/NursingHomeCompare/
After entering your location and getting info on a specific
facility, click on "Quality Measures" and scroll to the last
item in the table, but caveat: Take this info with several grains of sand.
|